Americans are well known around the world for having a significant issue with obesity as shown on this graphic from the National Institutes for Health:
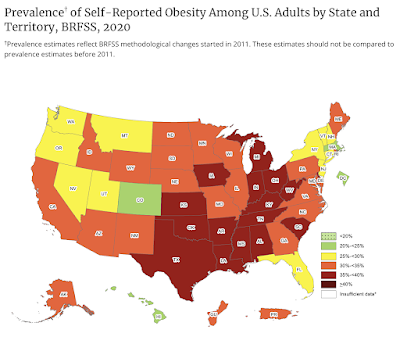
...and this graphic from the CDC:
...and this graphic which lists national obesity rates by nation:
When it comes to childhood obesity in the United States, we find this:
"For children and adolescents aged 2-19 years in 2017-2018:
The prevalence of obesity was 19.3% and affected about 14.4 million children and adolescents.
Obesity prevalence was 13.4% among 2- to 5-year-olds, 20.3% among 6- to 11-year-olds, and 21.2% among 12- to 19-year-olds. Childhood obesity is also more common among certain populations.
Obesity prevalence was 25.6% among Hispanic children, 24.2% among non-Hispanic Black children, 16.1% among non-Hispanic White children, and 8.7% among non-Hispanic Asian children.
With that background, let's look at the aforementioned research. We are now well aware of how governments used lockdowns to prevent the spread of the SARS-0CoV-2 virus and the fact that these lockdowns had a significant negative impact on individuals' mental and physical health. Let's look at a recent study on the CDC website which examines how the body mass index for children was impacted during the pandemic thanks to school closures, household income disruptions which resulted in changes to household food purchases, increased stress, increased screen time and fewer options for physical exercise:
The report opens by explaining the database used in the study. Data were obtained from IQVIA's Ambulatory Electronic Medical Records database and were used to compare longitudinal trends in body mass index (BMI in kg/m2) among a cohort of 432,302 young Americans between the ages of 2 and 19 years. Data from the pre-pandemic period from January 1, 2018 to February 29, 2020 was compared to data from March 1, 2020 to November 30, 2020. To qualify, children had to have at least two BMI measurements including one from prior to the pandemic and one during the pandemic with the pandemic measurement falling after the first three months of the pandemic (i.e. after May 31, 2020). Here is what the authors found:
1.) Prior to the pandemic, obesity prevalence was 16.0 percent including 4.8 percent with severe obesity. The monthly rate of BMI increase nearly doubled during the pandemic period when compared to the prepandemic period and the rate of change in the proportion of children with obesity was 5.3 times as high during the pandemic (0.37 percenctage point increase per month) than before the pandemic (0.07 percentage point increase per month). The estimated proportion of obese children rose from 19.3 percent in August 2019 and 22.4 percent in August 2020.
2.) Children in all BMI categories (excluding those who were underweight) experienced significant increases in the rate of BMI change, increase in body weight per month and over a six month period during the pandemic as follows:
a.) overweight - 2.13 times
b) moderately obese - 2.34 times - gain of 1.0 pounds per month with total gain of 6.1 pounds
c.) severely obese - 2.00 times - gain of 1.2 pounds per month with total gain of 7.3 pounds
This compares to a 2.7 pound weight gain over six months for a child with a healthy body weight prior to the pandemic.
3.) When looking at age ranges, children between the ages of 6 and 11 years saw the greatest increase in their rate of BMI increase at 2.5 times the prepandemic rate of increase. As well, the more obese that a child was, the higher the increase in their rate of BMI increase.
While it may seem relatively insignificant, the fact that the response to the pandemic resulted in significant increases in body weight for American children is of great concern for the future state of their health since childhood obesity is likely to result in adults with obesity as shown here. Accelerated weight gain among the already obese can put these children at risk for future health conditions including type 2 diabetes, hypertension, heart disease and depression. Thanks to government responses to the lowest risk cohort for severe and deadly COVID-19 infection outcomes, public health and elected officials may have traded one health problem for another, yet another unintended consequence of government ineptitude. Instead of being so fixated on getting every child vaccinated, public health should be concerned with childhood obesity which can lead to lifelong and serious health problems.









No comments:
Post a Comment